Several recent studies show that nuclear medicine breast imaging (also called scintimammography) may be useful as a supplement to mammography in helping to detect breast cancer. While mammography is the most effective tool for screening for breast cancer in women who do not show any signs of the disease (such as a lump), its sensitivity can be reduced in women with dense breast tissue. Nuclear medicine, when used in conjunction with mammography in evaluating breast abnormalities, may confirm the existence of breast cancer, rule out the possibility of cancer, or find breast cancer that has spread to the nearby lymph nodes.
Dense breast tissue is common in young women and makes the results of mammography more difficult to interpret. This is because breast density shows up as white areas on mammogram films, just as cancer does. Therefore, women are not recommended to begin annual screening mammography until they reach 40 years of age. However, some younger women at high risk of breast cancer may need earlier screening to help detect breast cancer when it is still easily treatable. For years, researchers have been investigating tests that can increase the accuracy of breast cancer detection in young women.
In a recent study conducted by Italian researchers,(1) mammography and nuclear medicine breast imaging were compared in 134 women aged 32 to 78. While the overall accuracy of the two tests were similar, mammography was less likely to identify breast cancer in the younger women than the nuclear medicine test. This suggests that nuclear medicine may be effective in women with dense breast tissue. The researchers concluded that nuclear medicine may help in surgical planning because of its high specificity and could be considered complimentary to mammography, especially in younger women. A Turkish study(2) also found that nuclear medicine breast imaging may be helpful in detecting breast cancer that had spread to the axillary (armpit) lymph nodes. In fact, nuclear medicine imaging is sometimes used with sentinel lymph node biopsy to help determine if the lymph nodes contain cancer cells.
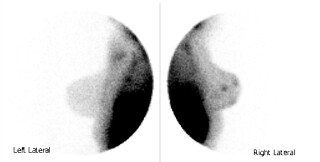
Nuclear medicine breast image.
In another study by researchers from the Los Robles Regional Medical Center in California,(3) nuclear medicine breast imaging was evaluated in 75 patients with signs on either mammography or physical exam that might or might not have indicated breast cancer. Of the 30 diagnosed cancers, 27 were positively identified with nuclear medicine. Eight of those 27 cancers were not identified with mammography or physical exam, and 11 of the cancers were smaller than one centimeter. The researchers concluded that nuclear medicine is a useful method of evaluating patients with indeterminate (difficult to read) mammograms or physical exams and may help detect additional small breast tumors.
However, not all studies indicate that nuclear medicine is a useful breast imaging test for small abnormalities. Other research has shown that nuclear medicine is only 40% to 60% accurate at imaging small breast abnormalities but more than 90% accurate in detecting abnormalities over one centimeter. However, mammography and physical exams are also very useful for detecting large abnormalities. It is the small abnormalities that tend to need additional imaging. Therefore, in this respect, nuclear medicine breast imaging may sometimes be of limited value.
To perform a nuclear medicine test, a radioactive tracer (Tc-99m sestamibi) is injected in the patient’s arm opposite of the breast being studied. The radioactive tracer travels throughout the body, including to the breast that needs to be imaged. Normal tissue will only accumulate a small amount of the radioactive tracer (dye). However, cancer cells tend to take up more of the dye. After the radioactive tracer has been injected, the patient is instructed to lie face down on a special table while the breast hangs down through an opening in the table. At this time, a special gamma camera is used to capture images of the breast from several angles.
While researchers continue to investigate the possible benefits of nuclear medicine breast imaging, the test is currently available for a small number of patients when further imaging is needed to investigate a breast abnormality. Nuclear medicine breast imaging is not available for breast cancer screening. Mammography has been shown to detect approximately 85% of all breast cancers and is considered the "gold standard" in breast cancer detection. Magnetic resonance imaging (MRI) has also shown promise in detecting breast cancer in some younger women with dense breasts, but further research is needed to determine its full benefits.
- (1) The study, "Sestamibi Scintimammography in pT1 Breast Cancer: Alternative or
Complementary to X-ray Mammography," is published in the May 2001 issue of Anticancer
Research. An abstract of the study is available at http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&
db=PubMed&list_uids=11501847&dopt=Abstract - (2) The study, "Role of Technetium Tetrofosmin Scintimammography in the Diagnosis
of Malignant Breast Masses and Axillary Lymph Node Involvement: A Comparative Study with
Mammography and Histopathology," is published in the December 1999 issue of the European
Journal of Surgery. An abstract of the study is available at http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&
db=PubMed&list_uids=10636548&dopt=Abstract - (3) The study, "Scintimammography in Patients with Minimal Mammographic or Clinical
Findings," is published in the May 2001 issue of Radiographics. An abstract of
the study is available at http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&
db=PubMed&list_uids=11353112&dopt=Abstract - To learn more about nuclear medicine breast imaging, please visit http://www.imaginis.com/breasthealth/nuc_med.asp
- To learn more about mammography, please visit http://www.imaginis.com/breasthealth/mammography.asp



