An aortic aneurysm is the bulging of a portion of the aortic wall. Aortic aneurysms are believed to be caused by the gradual weakening of the artery due to atherosclerosis, arterial narrowing and hardening from cholesterol plaque build-up. Other causes include hypertension (high blood pressure), Marfan syndrome (genetic connective tissue disease), infectious diseases such as syphilis or tuberculosis, or possibly a genetic predisposition in the case of abdominal aortic aneurysm.
Abdominal aneurysms are most common form of aortic aneurysm, comprising 75% of cases. Abdominal aneurysms are most often seen in men aged 40 to 70. Patients may also suffer thoracic aneurysms (in the chest cavity). Aortic aneurysms may be further classified as either fusiform (the aneurysm bulges in equal proportions and tapers at the ends, often seen in the lower abnormal aortic section) or saccular (the aneurysm bulges in only a portion of the aortic wall, often seen above the heart).
The rupturing of an aortic aneurysm is a life-threatening condition that requires immediate attention to prevent considerable internal bleeding, which may result in death. The risk of rupture is high if the abdominal aneurysm is more than four centimeters or the thoracic aneurysm is less than six centimeters. Another condition, an aortic dissection, occurs when a portion of the aortic lining tears. Aortic dissection accompanies aortic aneurysm in some cases. The risk of rupture from aortic dissection is more substantial than from aortic aneurysm.
Aortic aneurysm may or may not be accompanied by symptoms, including:
- Swelling or pain in the abdomen or lower back; may be severe if the aneurysm has ruptured (with abdominal aneurysm)
- Neck or back pain (with thoracic aneurysm)
- Cough, hoarseness or difficulty swallowing (with thoracic aneurysm)
- Chest pain (with thoracic aneurysm, may be mistaken for myocardial infarction)
- Swelling of neck or arms (with thoracic aneurysm)
- Dramatic decrease in blood pressure
- Nausea or blurred vision
Diagnosing an aortic aneurysm typically begins with a physical examination and blood pressure test. Careful documentation of family and medical history should also be noted at this time. Additional exams to test or confirm aortic aneurysm include:
- Echocardiogram (heart ultrasound): This diagnostic technique is an excellent tool to provide details of the cardiac structures – vessels, valves, and muscle. Echocardiography is a non-invasive exam in which images are acquired and viewed in real time without the use of radiation. Echocardiography is often useful in studying the beating heart and provides some information on functional abnormalities of the heart wall, valves and blood vessels. Echocardiography with Doppler is used to measure blood flow across valves, across septal defects (shunts), extent of regurgitations, etc. Color flow mapping capability is extremely useful in the detection of shunts. Abnormal operation of the valves can be detected by studying the opening and closing function versus normal valve function. Echocardiography may also be used to study congenital heart defects such as a septal defect (a hole in the wall that separates the two chambers of the heart).
- Chest x-ray: A chest x-ray images the heart and surrounding thoracic anatomy, shows heart size and shape, and reveals whether the heart is misshapen or enlarged due to disease. Abnormal calcification (hardened blockage due to cholesterol build up) in the main blood vessels and fluid in the lungs (possible indication of congestive heart failure) can also be seen. Chest x-rays can also be used to image pacemakers and artificial heart valves to check for correct positioning.
- Cardiac magnetic resonance (MR): Magnetic resonance (MR) imaging of the heart is a unique application that can provide valuable information in certain situations. Cardiac MR provides non-invasive imaging of the heart. Ultra-fast 2D and 3D imaging techniques coupled with the latest MR hardware now allow improved diagnosis in as little as a single breath-hold. New techniques are also being developed which allow first pass perfusion imaging of the heart. Cardiac MR applications and techniques are continuously improving and their use varies from center to center. However, cardiac MR applications appear to be very promising and may provide an excellent means to diagnose a number of heart conditions without requiring the use of x-rays or contrast injection, as with conventional x-ray angiography.
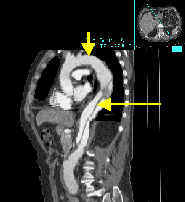
- Fast/multi-slice CT scan: Fast/multi-slice spiral CT scan with ECG gating is a new non-invasive method of imaging the heart and coronary arteries. In some cases, ECG gated fast/multi-slice CT eliminates the need for conventional cardiac angiography which requires invasive catheterization. Fast/multi-slice CT is particularly useful in that it can show calcium deposits in the coronaries that form with plaque-build up and may eventually lead to myocardial infarction (heart attack). Early imaging of stenoses (narrowing or arteries) and calcium deposits in the coronary arteries can allow aggressive preventive measures or treatment to be implemented, thus lowering the risk of myocardial infarction.